Figuring out how your genes and environment increase your likelihood of developing asthma, heart disease, cancer, dementia, and other conditions can have life-changing consequences. The field of genomics has made it relatively straightforward to test both in the hospital and at home for a wide range of genetic variations linked to disease risk.
In recent years, science has been making progress in tracking down the environmental culprits that drive risk for several diseases – and in identifying ways to optimize treatments based on your environmental exposures.
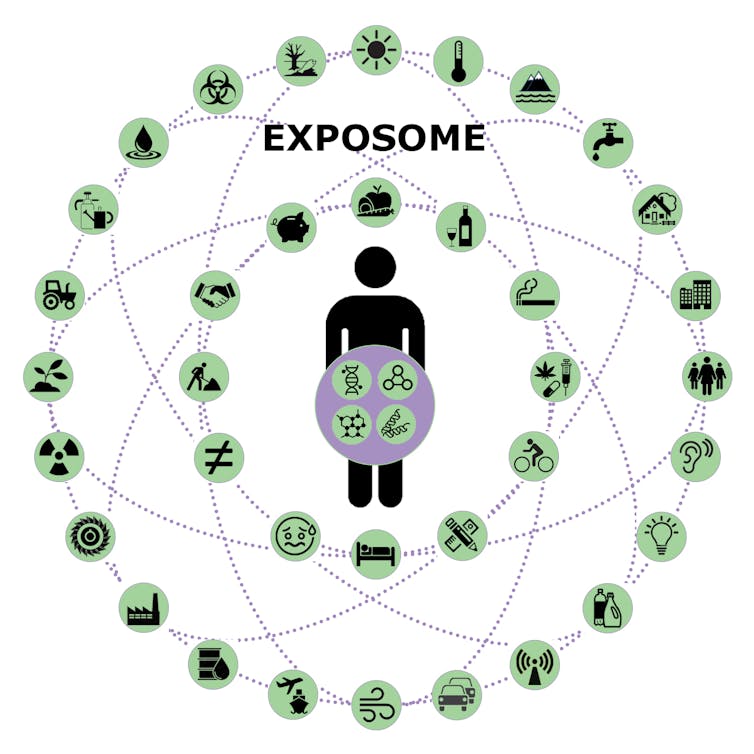
My work as a pharmacologist and toxicologist has led me to the emerging science of exposomics – the study of all of the physical, chemical, biological, and social factors that affect your biology. While your genome comprises all of the genes that encode your biology, your exposome is a concept that comprises all your environmental exposures. Like how researchers use DNA sequencers to study genomics, scientists in exposomics use chemistry and high-tech sensors to measure the effects of thousands of environmental factors on health.
Medications don’t always work.
For many people, standard drug therapies to treat certain conditions simply don’t work. Controlling blood pressure often requires months of trial and error. It can take months or even years to identify an adequate treatment plan for depression.
Adverse events caused by medications account for more than 1 million visits to emergency departments each year in the United States. What drives these differences in drug effects between patients? Is it their genes? Are they not taking their medication as prescribed due to side effects? Or something else?
As it turns out, your environment can have a major effect on how well specific treatments work for you. Think about the warning labels advising you not to drink grapefruit juice while taking a specific drug, for example. This is because a natural chemical in grapefruit inhibits the enzymes that break down those medications. Some common statins used to control high cholesterol can build up to toxic levels because the chemical in grapefruit juice blocks its normal processing.
Grapefruit isn’t the only environmental factor affecting how you respond to your medications. Over 8,600 chemicals are used in commerce in the United States, and you are exposed to thousands of these chemicals daily. It is more likely than not that many of these chemicals can interact with the drugs you take.
Some of the chemicals we use to keep fleas and ticks off pets can increase the levels of the same enzyme blocked by grapefruit juice, meaning a statin may be broken down so fast that it doesn’t control elevated cholesterol.
Byproducts from the combustion of organic matter, such as engine exhaust and burning wood, can also interfere with drug-metabolizing enzymes. Some of these chemicals, called polyaromatic hydrocarbons, can inactivate medications used to treat asthma. The environmental factor triggering your asthma could prevent the drugs used to treat it from working.
A chemical solution?
Advances in chemistry are helping researchers figure out what chemicals are getting in the way of treatment. Your hospital laboratory can already measure dozens of molecules in your blood. Measuring your salt levels can tell doctors how your kidneys are working, cholesterol levels indicate your risk of heart disease, and specific enzymes reveal your liver’s health. These common tests are routine and useful for nearly every patient.
Many additional tests can help determine how a specific condition is progressing or responding to therapy. Hemoglobin A1c levels help determine how well glucose levels are being controlled in those with prediabetes or diabetes. And thousands of other human diseases have their corresponding biomarkers.
In research laboratories, scientists can detect the presence of thousands of molecules at once using instruments called mass spectrometers. Each chemical in a sample has a unique mass, and these devices measure these masses for scientists to categorize.
Thus, scientists can identify all of the pesticides, plasticizers, plastics, pollution, and other chemicals present in a given sample. They can also measure your internal biology, such as the compounds involved in processing the food you eat and the hormones influencing how you behave.
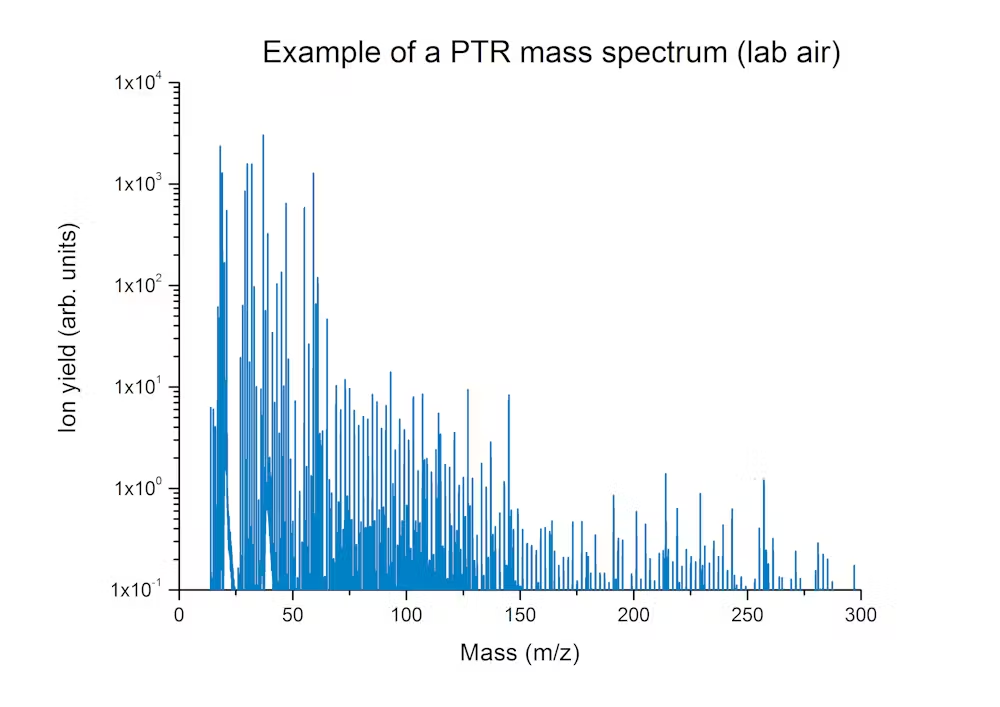
Taking all these factors together, scientists can study how your environment may be interfering with the effectiveness of your medications.
A better prescription – for you
Together with dozens of scientists across many institutions, my colleagues and I are developing methods to measure all of the chemicals in your body. The project, dubbed IndiPHARM – short for individualized pharmacology – is designing tools to measure a wide range of drugs, drug metabolites, and environmental chemicals at the same time.
By combining environmental data with genetic information, we hope to improve how drugs work in people by figuring out whether chemicals in their environment or diet are altering how they process a given drug. This includes whether the administered drugs are at therapeutic levels, how the drugs and chemicals are interacting with each other, and determining whether other variables are affecting intended drug effects. This could lead to changing the amount of drug prescribed, switching to a different medication or even redesigning the medicines themselves.
Our team is starting with identifying the environmental and biological factors associated with metabolic diseases, including obesity and diabetes, along with common co-occurring conditions such as hypertension, high cholesterol, and depression. For example, there are significant differences in how well people respond to anti-obesity or anti-diabetes drugs, and we hope to figure out why that is so all patients can benefit through tailored treatment.
Getting the right drug to the right person at the right time requires a better understanding of the environmental factors that influence how they work. We envision a future where a doctor can use your genetic and environmental history to determine the best drug treatment that would work for you from the start, reducing the need for trial and error.![]() _______________________________________________________________________________________________
_______________________________________________________________________________________________
Gary W Miller is a Professor of Environmental Health Sciences at the Columbia University Mailman School of Public Health.
This article is republished from The Conversation.
